Did you know that one in every 20 nursing home residents will develop pneumonia each year? This surprising statistic highlights why pneumonia in nursing home residents is a critical issue that too often goes unnoticed. Pneumonia is not only a leading cause of hospitalization and death in long-term care settings, but its subtle signs can be easily missed. Whether you are a concerned family member, a vigilant caregiver, or a healthcare professional, recognizing the warning signs early could mean the difference between recovery and serious complications. This guide unpacks everything you need to know to safeguard your loved ones—including risk factors, early symptoms, prevention strategies, and actionable steps for protection.
Pneumonia in Nursing Home Residents: The Overlooked Threat in Long-Term Care
A startling 1 in 20 nursing home residents will develop pneumonia each year, making it one of the leading causes of hospitalization and death in long-term care facilities. Discover essential information and actionable steps to safeguard loved ones.

Key Knowledge: What You’ll Learn About Pneumonia in Nursing Home Residents
How to recognize early signs and symptoms of pneumonia in nursing home residents
Critical risk factors and how to reduce them in nursing home settings
The latest diagnostic and treatment protocols for acquired pneumonia in older adults
Best practices to prevent respiratory infection outbreaks in nursing homes
Understanding Pneumonia in Nursing Home Residents: A Leading Respiratory Infection
Defining Pneumonia in Nursing Home Residents
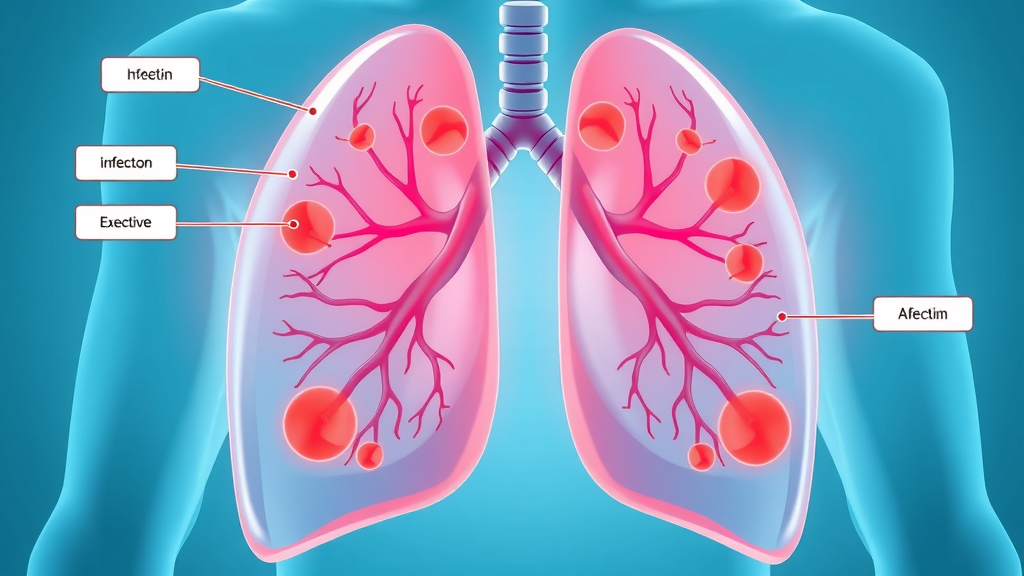
Pneumonia is a respiratory infection that inflames the air sacs in one or both lungs. For nursing home residents, especially those in long-term care, pneumonia can present unique challenges. Unlike the general population, these older adults often face weakened immune systems and multiple comorbidities, which increase their risk for acquired pneumonia. Nursing home residents are more likely to develop severe or atypical forms of pneumonia, including aspiration pneumonia , due to swallowing difficulties or limited mobility. Understanding the specific ways pneumonia develops in the nursing home setting is crucial for early detection and effective intervention.
The mechanism behind pneumonia in home residents involves exposure to bacteria, viruses, or other pathogens that the body can no longer fight effectively. Streptococcus pneumoniae is a common culprit, but gram-negative bacteria and viruses also challenge older adults. The term “nursing home-acquired pneumonia” differentiates these infections from community-acquired forms and highlights the unique risk factors faced by this vulnerable group. Early recognition, diagnosis, and intervention are essential for improved outcomes.
Prevalence and Impact of Respiratory Infections in Nursing Home Settings
Pneumonia is one of the most common and deadly respiratory infections in nursing homes, leading to countless hospital admissions and high mortality rates. Statistics reveal that up to 18% of deaths in long-term care are related to lower respiratory tract infections , making proper awareness a matter of life and death. The communal nature of long-term care facilities allows infections to spread rapidly, with older adults’ immune systems often unable to mount a strong defense. This makes prompt recognition and strict infection control vital.
The burden of pneumonia in home settings also extends to extended hospital stays, declining overall health, and increased healthcare costs. Many residents with advanced age or chronic diseases never fully recover baseline functioning after a severe respiratory infection, underscoring the need for aggressive prevention and intervention strategies. Staff shortages, shared living spaces, and high rates of underlying disease amplify the risk, making multidisciplinary care and heightened family engagement essential for protecting at-risk older adults.
Critical Risk Factors for Acquired Pneumonia Among Nursing Home Residents
Comorbidities and Immune System Challenges in Older Adults
One of the most significant risk factors for pneumonia in nursing home residents is the presence of multiple chronic illnesses or comorbidities. Conditions such as diabetes, heart disease, chronic kidney disease, and especially pre-existing lung diseases weaken the body’s defenses against infection. With age, the immune response also naturally declines, reducing the ability to fight off even common respiratory tract infections. This immune compromise means that infections, once established, progress more rapidly and are harder to treat than in the general population.
The cumulative effect of these health issues, particularly in long-term care environments, increases the likelihood that an older adult will acquire pneumonia. Additionally, use of medications that suppress immune function or impact swallowing can further increase the danger. Proactive monitoring, routine medical reviews, and close collaboration between care teams, families, and physicians can help lower this significant risk factor.
Aspiration Pneumonia in Nursing Homes: A Distinct Threat
Aspiration pneumonia is a specific and common threat in nursing homes, caused when food, liquid, or saliva enters the airways instead of the esophagus. This problem is particularly frequent among nursing home residents with neurological impairments, such as stroke or advanced dementia, or those with swallowing difficulties. Unlike traditional bacterial pneumonia , aspiration pneumonia can be harder to diagnose and presents with less typical symptoms, making vigilance vital in the nursing home setting.
The risks associated with aspiration pneumonia in term care cannot be overstated. Even small, repeated episodes of aspiration—especially in residents who are not fully upright during feeding—can quickly lead to severe lung infections. Caregivers and staff must be trained to identify swallowing difficulties, adjust feeding protocols, and intervene early to prevent progression from episodic aspiration to full-blown pneumonia. Simple measures, such as using thickened liquids and ensuring proper feeding positions, can make a life-saving difference.

Environmental and Procedural Risk Factors in Long-Term Care Facilities
The design and operation of long-term care facilities directly influence the risk of acquired pneumonia. Crowded common areas, poor ventilation, inadequate cleaning, and shared equipment all contribute to the rapid spread of infectious disease. When infection control practices fall short or staff members are undertrained, these environmental risk factors create ideal conditions for outbreaks of respiratory infections. Regularly updating infection protocols and providing ongoing staff education are key measures to counter these risks.
Moreover, daily routines such as oral care, mobility practices, and feeding methods impact susceptibility. Residents who are bedridden or have limited mobility become more prone to aspiration and lung congestion, while lapses in oral hygiene increase the amount of bacteria that can enter the lungs. Nursing homes must ensure adequate staffing and provide resources for both routine preventive care and quick response to initial symptoms of illness.
The Influence of Respiratory Tract Infections and Underlying Diseases
Pre-existing respiratory tract infections or recurrent illnesses significantly heighten the threat of pneumonia for nursing home residents. Older adults with a history of recurrent bronchitis, COPD, or other lower respiratory tract illnesses face a compounded risk due to already compromised lung function. The presence of multiple underlying diseases, coupled with weakened natural defense mechanisms, can turn minor respiratory symptoms into life-threatening conditions remarkably quickly.
Understanding these pathways empowers both staff and family members to escalate care at the first sign of a respiratory issue. Engaging physicians in the early evaluation of any suspected tract infection and maintaining regular monitoring are essential parts of a successful prevention and intervention plan for this highly vulnerable population.
Warning Signs: How to Identify Pneumonia in Home Residents Early
Common initial symptoms: fever, cough, and changes in mental status
Subtle and atypical presentations: In older adults, pneumonia may present as confusion, sudden decline in function, lack of appetite, or increased falls, without classic signs like fever or productive cough.
Importance of chest radiograph findings and diagnostic strategies: Chest x-rays (radiographs) remain a gold standard for confirming pneumonia in nursing home residents. Imaging is essential when symptoms are unclear or progress quickly.

“Prompt recognition of pneumonia symptoms in nursing home residents can literally save lives.” — Infectious Diseases Society of America
Diagnosing Pneumonia in Nursing Home Residents: Tools and Protocols
Physical Assessment and Symptom Review
The diagnostic journey for pneumonia in nursing home residents begins with a thorough review of symptoms and a complete physical assessment. Common clues include increased or productive cough, fever, chills, shortness of breath, and new difficulties with daily activities. However, older adults often exhibit non-specific symptoms such as confusion, sudden functional decline, or worsening chronic conditions. Because these symptoms can overlap with other illnesses, healthcare staff in the nursing home setting require training to assess subtle shifts in behavior and alertness.
Additionally, vital signs—such as elevated temperature, rapid breathing, or low oxygen saturation—warrant urgent follow-up. Nurses and care teams should use checklists to document changes promptly and share findings with medical providers to speed up diagnosis and treatment. In cases where pneumonia is suspected but initial symptoms are mild, close monitoring is vital for early intervention.
Role of Chest Radiography and Modern Imaging in the Nursing Home Setting
Chest radiography (chest x-ray) plays an essential role in confirming suspected pneumonia in nursing home residents. While some facilities are equipped to perform bedside imaging, others may transfer residents to a clinic or hospital for a chest radiograph. The x-ray can reveal classic signs of lower respiratory tract infection like lung infiltrates or consolidation, which are not always present in the earliest stages or in frail residents. Advanced imaging such as CT scans may be used if the diagnosis remains uncertain, especially in complex cases involving comorbidities or suspected aspiration pneumonia.
Rapid interpretation of imaging studies enables prompt and targeted treatment, helping decrease the risk of severe complications or the need for hospitalization. Efforts to bring portable radiography equipment into long-term care settings are increasing, minimizing disruptions for residents and allowing timelier diagnoses.

Laboratory and Microbiological Testing for Accurate Diagnosis
Besides clinical evaluation and imaging, laboratory tests—such as blood counts, C-reactive protein, and pulse oximetry—offer valuable clues about the severity of infection. Microbiological testing might include sputum samples or nasopharyngeal swabs to identify bacterial or viral pathogens responsible for the respiratory infection. Understanding the exact cause of pneumonia in a nursing home resident is essential for selecting the most effective treatments and for implementing infection control if an outbreak is likely.
In the nursing home setting, delays in sample collection or result reporting can hamper timely care. Thus, having a clear protocol for evaluation and a collaborative approach between care staff, laboratory technicians, and clinicians can make diagnosis markedly more efficient and improve outcomes for at-risk residents.
Comparison of Pneumonia Symptoms in Nursing Home Residents vs. Older Adults in Home Settings
Symptom |
Nursing Home Residents |
Older Adults in Home Settings |
|---|---|---|
Fever |
Often mild or absent |
Typically present |
Cough |
May be non-productive; less noticeable |
Productive, prominent symptom |
Confusion/change in mental status |
Very common and may precede respiratory symptoms |
Less frequent, usually after onset of fever/cough |
Breathing difficulties |
Often subtle or gradual onset |
Rapid or sudden onset |
Treatment Approaches: Managing Acquired Pneumonia and Respiratory Infections in Nursing Homes
Antibiotic Therapy: Recommendations and Guidelines from the Infectious Diseases Society of America
The mainstay of pneumonia management in nursing homes is antibiotic therapy —tailored to the likely pathogen, severity of illness, and local resistance patterns. The Infectious Diseases Society of America (IDSA) recommends prompt initiation of antibiotics, with choices often including oral or intravenous cephalosporins, macrolides, or fluoroquinolones, depending on clinical context. Rapid, appropriate antibiotic selection—guided by established protocols—can curb progression to severe disease and limit the risk of secondary lower respiratory tract infections.
Antibiotic therapy is monitored closely for effectiveness, with clinicians watching for improvement in fever, cough, breathing, and overall status within 48-72 hours. Switching or modifying therapy may be needed if residents do not respond as expected or if cultures reveal resistant bacteria.

Supportive Care and Oxygen Therapy for Elderly Residents
Beyond antibiotics, supportive care is a cornerstone for treating pneumonia in nursing home residents. This includes supplemental oxygen for hypoxia, intravenous fluids for dehydration, and respiratory therapy if airway clearance is compromised. Many older adults are at high risk for complications from even mild fluid or oxygen imbalances, so diligent nursing assessment and frequent adjustments are crucial. Chest physiotherapy, mobilization, and nutritional support all contribute to a more complete recovery.
Families and staff play a vital role in ensuring that residents are positioned comfortably, can access needed mobility aids, and receive regular mouth care to minimize the risk of lower respiratory tract infection recurrence. Proactive pain management, prevention of pressure ulcers, and early treatment of secondary infections are other important aspects of supportive care in a long-term care environment.
Addressing Complications and Preventing Lower Respiratory Tract Infections
Pneumonia often leads to complications such as respiratory failure, sepsis, and worsening cognitive or physical function. Early intervention and close observation can help prevent these outcomes, but once complications develop, more aggressive interventions—including hospital transfer or palliative care—may become necessary. Preventive measures, such as swallowing assessments and routine oral hygiene protocols, help reduce recurrence rates and lower the overall burden of disease in the facility.
Addressing these issues requires communication between clinical staff, residents, and families to ensure that interventions align with the resident’s wishes and advance care plans. Ongoing staff training on best practices for aspiration prevention, infection monitoring, and complication recognition is key to lowering rates of hospital readmissions and improving long-term outcomes.

Managing Infectious Diseases and Protecting Other Residents
In the communal nursing home setting , containing the spread of infectious disease is a top priority. Rapid identification and isolation of affected residents—combined with strict hand hygiene and use of personal protective equipment—can prevent large outbreaks of acquired pneumonia. Staff education, ongoing training, and transparent communication with families about infection control protocols foster trust and cooperation for best outcomes.
Engaging residents in flu vaccine campaigns, reinforcing cough etiquette, and regular screening for early symptoms all contribute to a safer environment for both residents and staff. The ultimate goal is to break the chain of transmission and protect all vulnerable individuals within the nursing home community.
Prevention Strategies for Pneumonia in Nursing Home Residents
Vaccinations: Influenza and pneumococcal immunizations are essential for all nursing home residents and staff. Staying current greatly reduces the risk of severe respiratory infection.
Staff education and infection control: Ongoing training for caregivers in recognizing early warning signs, practicing proper hand hygiene, and using personal protective equipment.
Proper oral care and feeding practices: Daily mouth care, careful feeding of high-risk residents, and early recognition of swallowing issues prevent aspiration pneumonia.
Monitoring and minimizing aspiration risk: Conduct regular swallowing assessments, use thickened liquids when appropriate, and position residents upright during and after meals.
Role of Nursing Home Staff and Families: Advocating for At-Risk Older Adults
How Vigilant Caregivers Can Reduce Respiratory Infection Risk Factors
Caregivers are the first line of defense against respiratory tract infection in the nursing home environment. Observing subtle shifts in a resident’s behavior, breathing, or appetite—and promptly communicating these changes to healthcare providers—can halt pneumonia in its earliest stages. Ongoing education about infection prevention practices, symptom monitoring, and thorough documentation empowers staff to swiftly identify and address all risk factors.
Families, too, play a crucial role by staying actively involved, asking targeted questions, and ensuring that residents are not neglected. When families and staff work as a team, early escalation of minor health issues becomes routine, reducing the overall odds of severe acquired pneumonia and related hospitalizations.
Coordinating with Healthcare Teams for Early Intervention
Effective management of pneumonia in nursing home residents depends on consistent, open communication between nursing staff, physicians, therapists, and family members. Swift action on new or unusual symptoms—such as sudden confusion, cough, or unexplained weakness—ensures residents receive timely clinical evaluation and appropriate therapy. Coordination also extends to care conferences and advance planning for those with complicated medical backgrounds.
Engaging multidisciplinary teams and involving the resident’s family in all aspects of care planning is a proven strategy for catching respiratory infection early and ensuring all necessary supports are in place for recovery. Family involvement and advocacy are strong predictors of better outcomes in older adults facing the threat of pneumonia.
“Family involvement is a strong predictor of better outcomes in nursing home residents facing pneumonia.”
Legal and Ethical Considerations When Pneumonia Strikes Nursing Home Residents
Understanding Resident Rights and Facility Responsibilities
Nursing home residents and their families have legally protected rights to receive safe, appropriate, and timely medical care—including prevention, diagnosis, and treatment of respiratory infections like pneumonia. Facilities are required by law to maintain standards for cleanliness, staffing, infection control, and symptom monitoring. Failing to meet these obligations may be grounds for complaint or legal action, especially if poor care leads to avoidable harm.
Informed consent, shared decision-making, and clear documentation of all interventions are essential. Families should feel empowered to ask questions about care plans, treatment choices, and the facility’s readiness to recognize and manage infectious disease outbreaks. Advocacy for the resident’s wishes, including preference for hospitalization or palliative measures, is central to ethical care.

When Poor Care Leads to Pneumonia: Recognizing Signs of Neglect
Pneumonia cases that arise from neglect—such as failure to assist with feeding, delayed recognition of symptoms, or improper use of infection control practices—are unfortunately not rare. Family members and outside advocates should be vigilant for warning signs of substandard care, including unaddressed swallowing difficulties, lapses in oral hygiene, or overcrowded conditions. Documenting concerns, seeking medical opinions, and understanding the process of filing complaints or pursuing legal remedies are important steps when there’s suspicion that a loved one’s pneumonia was preventable.
Ethically, all individuals involved in long-term care have a duty to ensure the health and dignity of residents—especially when it comes to conditions as serious as acquired pneumonia. Pursuing accountability not only protects the individual resident but can drive wider improvements across the facility.
Essential Reminders: Quick Reference Checklists for Nursing Home Staff and Families
Immediate actions when warning signs appear
Daily routines to minimize acquired pneumonia risk
Key questions to ask the care team regarding respiratory infections

Frequently Overlooked Facts About Pneumonia in Nursing Home Residents
Not all coughs signal a respiratory infection
Pneumonia can progress more rapidly in nursing home settings
Regularly updating vaccines is crucial
“Pneumonia prevention in nursing homes is not just a medical duty, but a shared social responsibility.” — Society of America for Infectious Diseases
People Also Ask: What is the most common cause of pneumonia in nursing homes?
The most common cause of pneumonia in nursing homes is aspiration, where food, liquid, or vomit is inhaled into the lungs, often compounded by weakened swallowing reflexes in older adults. Bacterial respiratory infections, particularly from Streptococcus pneumoniae and gram-negative bacteria, are leading infectious culprits in long-term care settings.
People Also Ask: How do nursing homes treat pneumonia?
Nursing homes treat pneumonia in residents using a combination of antibiotic therapy according to the latest guidelines, supportive treatments such as oxygen and intravenous fluids, and close clinical monitoring. Early intervention and isolation may be employed to prevent the spread of acquired pneumonia and respiratory infections.
People Also Ask: What is the end stage of pneumonia in the elderly?
In elderly nursing home residents, the end stage of pneumonia can involve severe difficulty in breathing, dehydration, multi-organ dysfunction, and, tragically, can be life-limiting. Palliative approaches may be prioritized to ensure comfort, especially in those with multiple comorbidities.
People Also Ask: Can you sue a nursing home for pneumonia?
You may pursue legal action against a nursing home if negligence or substandard care contributed to a pneumonia diagnosis in a resident. This may include lack of timely care, poor infection control, or failure to monitor and respond to known risk factors. Documentation and expert guidance are recommended.
Best Practices Checklist for Preventing Respiratory Infections and Acquired Pneumonia in Nursing Homes
Ensure all nursing home residents receive recommended vaccines
Promote regular hand hygiene and respiratory etiquette
Implement staff training on early symptom recognition
Forward suspected cases to clinical evaluation rapidly
Maintain excellent oral hygiene routines for residents
Monitor for aspiration and address swallowing difficulties
Foster family engagement in care planning
Table: Summary of Risk Factors and Prevention Strategies for Nursing Home Residents
Risk Factor |
Prevention Strategy |
|---|---|
Advanced age |
Timely vaccinations, proactive health reviews |
Chronic diseases |
Regular assessment of comorbidities |
Swallowing impairment |
Managing feeding, use of thickened liquids |
Poor oral hygiene |
Daily dental care and staff training |
Staff shortages |
Adequate staffing and infection protocols |
Frequently Asked Questions Regarding Pneumonia in Nursing Home Residents
What are the signs of aspiration pneumonia in older adults? Look for coughing during meals, difficulty swallowing, sudden changes in breathing or oxygen levels, and confused mental status. Any of these symptoms in a nursing home resident with risk factors should prompt immediate clinical evaluation.
How often should chest radiographs be used in diagnosing respiratory infections? Chest x-rays are essential whenever pneumonia is suspected and help differentiate between other causes of symptoms. They should be utilized swiftly when initial signs or atypical changes occur.
Are there specific guidelines for antibiotic therapy in nursing home settings? Yes. The Infectious Diseases Society of America and similar authorities provide detailed recommendations on antibiotic choices, dosing, and monitoring specific to older and frail populations.
How can families monitor for early respiratory tract infections? Be alert for new cough, confusion, weakness, or change in baseline behavior, and communicate these immediately to staff and care providers for prompt assessment.
What long-term outcomes can nursing home residents expect after pneumonia? Recovery varies. Some return to prior health, while others suffer from persistent weakness or decline in function. Early intervention improves outcomes, but advance care planning is especially important in severe or recurrent cases.
What should be included in advance care planning discussions? Discuss preferred treatment approaches, desired level of intervention, wishes regarding hospitalization and comfort-focused care, and identification of surrogate decision-makers
Helpful Resources for Protecting Nursing Home Residents from Pneumonia
Infectious Diseases Society of America pneumonia guidelines
Centers for Disease Control and Prevention – Influenza and pneumonia resources
Local health department recommendations for nursing facilities
Staying Vigilant: How Families and Staff Can Make a Difference in Pneumonia Outcomes
By proactively addressing risk factors, staying informed about warning signs of pneumonia in nursing home residents, and working closely with clinical care teams, families and staff can significantly reduce preventable complications and protect vulnerable older adults.
Take action today—stay alert to symptoms, support preventive care, and advocate with healthcare teams to protect loved ones from the hidden dangers of pneumonia in nursing home residents.
Pneumonia is a significant health concern among nursing home residents, often leading to severe complications or even death. Understanding the risk factors and implementing effective prevention strategies are crucial in safeguarding this vulnerable population.
The article “Nursing Home-Acquired Pneumonia: Enhancing Care and Reducing Risks in Long-Term Care Settings” provides comprehensive insights into the risk factors associated with pneumonia in nursing homes, such as advanced age, chronic health conditions, and functional limitations. It also outlines preventive measures, including immunization, proper hand hygiene, and oral care, to mitigate these risks. (dovemed.com)
Additionally, the study “Pneumonia in residents of long-term care facilities: epidemiology, etiology, management, and prevention” delves into the prevalence and causes of pneumonia in long-term care settings. It emphasizes the importance of accurate diagnosis and tailored treatment plans to improve patient outcomes. (pubmed.ncbi.nlm.nih.gov)
For those committed to protecting nursing home residents from pneumonia, these resources offer valuable information on identifying risk factors and implementing effective prevention and management strategies.
Article provided by:
Kenneth D. St. Pé, APLC
Address: 700 St John St #401, Lafayette, LA 70501
Phone: (337) 534-4043
Website: stpelaw.com
Facebook: facebook.com/stpelawfirm
 Add Row
Add Row  Add
Add 



Write A Comment